Abstract
INTRODUCTION: Myeloproliferative neoplasms (MPNs) are clonal hematopoietic stem cell diseases characterized by the overproduction of differentiated myeloid cells. In classical BCR-ABL negative MPNs -essential thrombocythemia (ET), polycythemia vera (PV), prefibrotic primary myelofibrosis (prePMF) and overt myelofibrosis(MF) - driver mutations are described in JAK2, CALR and MPL genes. However, there is no compelling evidence to explain how each mutant gene can lead to phenotypically distinct and/or overlapping diseases, nor is it understood how additional gene aberrations modulate MPN phenotype. In an attempt to understand the molecular events that underlay clinical characteristics of MPNs, we sequenced hematopoietic cells of MPN patients with a focus on MF landscape.
METHODS: Patients were consented to MI-ONCOSEQ study approved by the University of Michigan IRB. MI-ONCOSEQ is a CLIA-certified Next Generation Sequencing (NGS) platform designed to identify genetic aberrations in a panel of 1,711 genes. MI-ONCOSEQ test can identify somatic point mutations, small insertions/deletions (indels), and copy number alterations by comparing the tumor sample (blood or bone marrow derived myeloid cells) to the matched normal sample (buccal swab or saliva derived normal cells). The assay also includes gene expression and gene fusion analysis of 24,774 capture targets based on transcriptome sequencing. Significant genetic variants were reported based on tumor burden in sample, as samples were collected at various stages of disease progression and treatment. Diagnoses of ET, PV, prePMF, or overt MF were confirmed by 2016 WHO classification as close to the time of sample collection as possible.
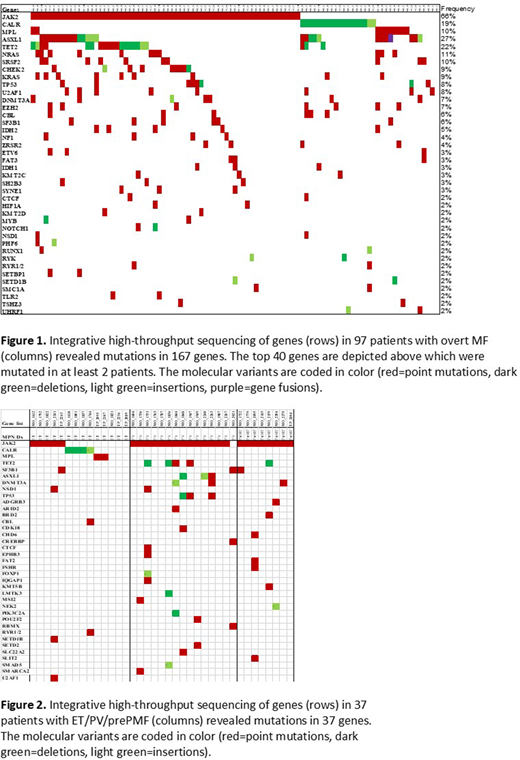
RESULTS: A cohort of 166 patients with suspected classical MPNs were enrolled, of which 32 were excluded from analysis due to diagnosis of other myeloid malignancy or a benign condition. Of the 134 evaluable patients, 97 (age range 33-84 yrs) were determined to have WHO-defined overt MF and 37 (age range 20-83 yrs) were determined to have WHO-defined ET, PV, or prePMF (14, 15, and 8, respectively). Most (95% of overt MF and 90% of ET/PV/prePMF) harbored driver mutations in JAK2, CALR, or MPL. In total, 167 genes were found to be mutated in 97 patients with overt MF (51 with primary MF, 46 with post-PV/ET MF) (Figure 1) as compared to only 37 genes in 37 patients with ET/PV/prePMF (Figure 2). There was a significant difference (p<0.0001) between the number of genetic variants in overt MF (4 per patient, range 0-9) as compared to ET/PV/prePMF (2 per patient, range 0-7). Of note, RAS pathway genes (NRAS, KRAS, and NF1) were found to be mutated only in overt MF (24% of cases) and not in ET/PV/prePMF. A comparison of genetic variant rate in ET to PV was also found to be significant (p<0.0007) 1 vs 3 variants per patient respectively, whereas prePMF presented a genetic variant landscape that was in between ET and PV. Both primary and post-PV/ET MF had the same average variant rate of 4 per patient.
CONCLUSIONS: To our knowledge, this is the largest integrative (NGS, gene expression, and transcriptome) sequencing study in patients with MPNs to date. Our results illustrate the following: 1) MF is likely an evolutionary disease arising from ET/PV/PrePMF by accumulating mutations, 2) RAS pathway activation might play a role in the transformation of ET/PV/PrePMF to overt MF and contribute to the proliferative nature of the disease, 3) Contrary to prior reports we observed an increasing mutation rate from ET < prePMF < PV < overt MF, 4) The aggressive nature of PV might be partly explained by a higher mutation burden compared to ET, 5) PrePMF displays an intermediate number of mutations which correlates with the clinical phenotype. Gene expression analysis to determine activated pathways and multivariate analysis to correlate clinical phenotype and gene to gene relationships are in progress.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal